Posted in Uncategorized
During the pandemic, the Centers for Medicaid and Medicare issued a Public Health Emergency (PHE). This meant that no one could be taken off of Medicaid during that time. It has been announced that on May 11, 2023 the PHE will be ending. The state of South Carolina began sending out Medicaid renewal forms beginning April 1 and has started the renewal process.
Here are three things you should do if you are on Medicaid today:
- If you have moved since the start of the pandemic (March of 2020), make sure the Medicaid agency has your most recent contact information.
Change online at apply.scdhhs.gov.
Call (888) 549-0820 Monday through Friday from 8am to 6pm
Or, you can visit your local eligibility office. - Check Your Mail
Be on the lookout for a renewal form (Annual Review) or any mail from the Medicaid office. - Complete Your Renewal From (if you get one)
Fill the form out to the best of your ability and return it to make sure your Medicaid coverage continues. The agency will contact you if more info is needed.
Frequently Asked Questions
The following are frequently asked questions about the renewal process
General Questions
Will Medicaid members lose their Medicaid health insurance as soon as the PHE ends (May 11)?
Medicaid renewals began April 1st, 2023. In SC, renewal notices will be sent out monthly over a 12-month period. Not all Medicaid members will receive a renewal form. Medicaid members who receive renewal notices will have 90-days to act. People can begin losing their Medicaid coverage as early as May 11, 2023.
Will all Medicaid members receive a renewal notice?
No. If the Medicaid office does a review and finds out a member is not eligible, the member will get a notice notifying them that they are no longer eligible. If you think that is wrong, then you can appeal and provide information that you think will prove you are still eligible.
If I am no longer eligible for Medicaid as a parent, does that mean my child(ren) will lose their coverage?
Your child might still be eligible because their eligibility has different income standards. Fill out the form with their information to try and keep them on Medicaid. Take action regardless of your situation!
If someone in my household is no longer eligible for Medicaid, does that affect the coverage of other household members?
You might still be eligible under another category and income. Take action regardless of your situation!
Who’s most at risk of losing Medicaid during this transition?
- Young people who have turned 19+ in the last 3 years and thus no longer qualify for Medicaid as children
- People who received Medicaid during their pregnancy but are past South Carolina’s postpartum eligibility coverage period (12 months postpartum)
- Part-time workers
- People with incomes close to the eligibility cutoff
- People with disabilities
What if members lose their Medicaid coverage?
We want all eligible South Carolinians to get and stay covered. If a member no longer qualifies for Medicaid health insurance, they will get:
- Notice of when their Medicaid coverage will end
- Information on how to request an appeal
- Information about the Health Insurance Marketplace (HealthCare.gov) and other affordable health care coverage options
- Members can visit HealthCare.gov or call the Marketplace Call Center at 1-800-318-2596 (TTY: 1-855-889-4325) to get details about Marketplace coverage
- If members need help applying for health insurance, Palmetto Project Insure-SC health insurance assisters may be able to help. Call (888) 998-4646 to schedule a free appointment.
Is the form available online in Spanish?
Currently only the mailed form is in Spanish if the family indicated they are Spanish-speaking. There is no web-version on the online form in Spanish currently. You may, however, call to complete your renewal with a Spanish speaker at 1-888-549-0820 (TTY: 1-888-842-3620).
What if members lose their Medicaid coverage–wrongful terminations?
If you think your Medicaid was cut off and this is wrong, ask for a fair hearing immediately. This will allow you to challenge the decision and provide information as to why this agency decision is wrong. If you win the Fair Hearing the agency must go back and pay your provider.
I lost my Medicaid coverage. Where can I get help?
If members need help applying for health insurance, Palmetto Project Insure-SC health insurance assisters may be able to help. Call (888) 998-4646 to schedule a free appointment.
What if members lose their Medicaid coverage–wrongful terminations?
How do I make an online account?
Check out this video from SCDHHS on how to make an online account to submit your renewal.
Filling Out the Form
WATCH: How to Complete the Form Online | In Spanish
IMPORTANT FOR ALL APPLICANTS
It is vital that you do two things when completing the form:
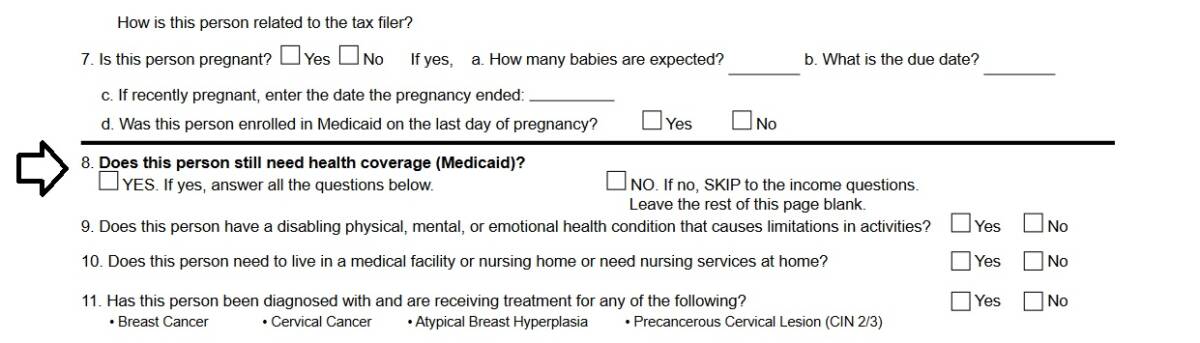
- Make sure you answer Question 8 in the Step 3 to identify that you want to continue Medicaid services
- Sign your form at the very end before submitting the form back to SCDHHS.
The agency cannot move forward on your application without these two questions answered.
I lost my renewal form, what should I do?
The best answer is to either call or go online to complete your form. Here’s how:
- Go online at apply.scdhhs.gov, or;
- Call 1-888-549-0820 (TTY: 1-888-842-3620) Monday through Friday from 8am to 6pm
- If you prefer completing a paper form, you may reprint a new copy here, but we encourage everyone to call or complete the form online if you do lose your form.
On Step 1, both address sections are blank. What should I do?
It’s okay! You can just add your current address to the right side of the form on Step 1.
My family member moved into my home in 2020/2021 and has been here for over a year. Should I include them in changes to your household even though it was longer than the past year?
Yes! Include everyone in your home on the Medicaid renewal form, especially if they are not included in the “Current Medicaid Household” list on your form. We want to make sure everyone in the home is accounted for in case they are eligible for Medicaid.
What is the point of an Authorized Representative?
An authorized representative may be a person that is helping you complete the form. The person is maybe a friend, relative, or acquaintance that you trust and give permission to help go through your records and keep up with your Medicaid account. It is not mandatory to have an Authorized Representative. You may leave the section blank.
Have more questions? Email us at [email protected] today.

